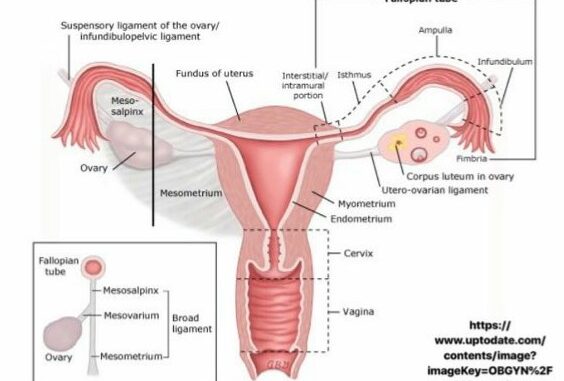
Cervix Anatomy
Cervix or cervix uteri is the lower part of the uterus, the human female reproductive system. It can be 2cm or 3m long but the length can change throughout pregnancy. It is narrow, cylindrical and runs along its entire length to connect uterus cavity and Vagina. Three most important parts of it are internal os which means its opening in a uterus cavity and external os which means its opening to the vaginal lumen and cervical canal which lies between internal and external os. A cervical canal is the passage through which, a sperm must travel to fertilize an egg cell after sexual intercourse.
Epidemiology
Cancer of the uterine cervix is the third most common gynecologic cancer diagnosis and cause of death among gynecologic cancers in the United States. In Rwanda, as the entire Easter Africa has one of the highest levels of mortality among cases of cervical cancer in the world and women in the region have a 2.7% cumulative probability of death from cervical cancer. According to the age-standardized estimates of the International Agency for Research on Cancer and the World Health Organization, in 2008 Rwanda had 34.5 cases of cervical cancer and 25.4 deaths attributable to cervical cancer per 100 000 inhabitants. At the time, the incidence of cervical cancer among Rwanda’s women appeared to be higher than the combined incidences of breast, liver and stomach cancer. Thanks to the tireless effort that Government of Rwanda has put into Vaccine against Human papilloma virus, which is the major causative agent of cervical cancer worldwide.Global incidence and mortality rates depend upon the presence of screening programs for cervical precancer and cancer and of human papilloma-virus (HPV) vaccination, which are most likely to be available in developed countries. Due to these interventions, there has been a 75 percent decrease in the incidence and mortality of cervical cancer over the past 50 years in developed countries. It is still a huge burden in low-income and middle income countries as preventive measures are not yet integrated in comprehensive women health care programs. As we all know low socio-economic status is the risk factor of getting this cancer.
What causes cervical cancer?
Human papillomavirus (HPV) is central to the development of cervical neoplasia and can be detected in 99.7 percent of cervical cancers. HPV plays a role primarily in the two most common histologic types of cervical cancer: squamous cell (69 percent of cervical cancers) and adenocarcinoma (25 percent). We know more than 40 genital mucosal HPV types identified, approximately 15 are known to be oncogenic where HPV 16 and HPV 18 are found in more than 70% of all cervical cancers. Most HPV infections are transient, and the virus alone is not sufficient to cause cervical neoplasia. When HPV infection persists, the time from initial infection to development of high grade cervical intraepithelial neoplasia and, finally, invasive cancer takes an average of 15 years, although more rapid courses have been reported.
Here are signs and symptoms of cervical cancer
Early cervical cancer is frequently asymptomatic, underscoring the importance of screening. The most common symptoms at presentation are irregular or heavy vaginal bleeding and postcoital bleeding. Though some women present with a vaginal discharge that may be watery, mucoid, or purulent and malodorous. This is a nonspecific finding and may be mistaken for vaginitis or cervicitis.
Advanced disease may present with pelvic or lower back pain, which may radiate along the posterior side of the lower extremities. Bowel or urinary symptoms, such as pressure-related complaints, hematuria, hematochezia, or vaginal passage of urine or stool, are uncommon and suggest advanced disease.
Screening, early detection and diagnosis
Screening in an otherwise, healthy immunocompetent woman is recommended starting by 21 years of age, reason being in this age group, women are sexually active and Chance of being infected by HPV (Human papilloma virus) is too high, many studies have shown that incidence of cervical cancer is too rare in younger women than 21years of age. Current protocol in the states and Rwanda recommend Starting at age 21, women should be screened even if they report sexual abstinence. Women may have a variety of reasons for not disclosing prior sexual activity, including social, religious, or cultural norms as well as reluctance to acknowledge prior sexual abuse or rape. In particular, women who have been sexually abused or raped are often reluctant to acknowledge this history, and abuse may underlie the decision to not engage in subsequent sexual activity.
We suggest screening women age <30 years with Papanicolaou (Pap) test alone at intervals of every three years. We suggest women age ≥30 years and older be screened with either: Pap test every three years, Co-testing (Pap test and HPV testing) every five years if both initial tests are negative.
Who are at risk of cervical cancer?
Early onset of sexual activity, risk is 1.5 fold for 18-20 years, two fold for those younger than 18 years.
Multiple sexual partners.
A high-risk sexual partner (eg: a partner with multiple sexual partners or known HPV infection)
History of sexually transmitted infections (eg, Chlamydia trachomatis, genital herpes)
Immunosuppression (eg, human immunodeficiency virus infection).
Smoking (for squamous cell carcinoma of the cervix).
Low socioeconomic status is associated with an increased risk of cervical cancer.
In contrast to squamous cell cancer of the cervix, cigarette smoking is not associated with a significantly increased risk of adenocarcinoma of the cervix compared with nonsmokers.
When to discontinue screening for cervical cancer?
In women aged 65 years or older provided that they have got prior adequate screening basing on 3 criteria
- No increased risk (i.e, history of abnormal screening, current smoker or history of smoking, unknown screening history, previous HPV-related disease, new partners, immunocompromised, in utero diethylstilbestrol exposure).
- Adequate prior screening: two negative consecutive co-tests or three negative Pap tests within the past 10 years, with the most recent test within the previous five years.
- No history of high-grade dysplasia or worse.
What is a Papanicolaou test?
The Pap test consists of cells sampled from the cervix and vagina. It can identify abnormal cells from the transformation zone and the junction of the ecto- and endocervix, where cervical dysplasia and cancers arise.
Diagnosis of cervical cancer
Diagnosis of cervical cancer consists of analyzing a tissue biopsy, mainly from the cervix. We have 3 histopathological diagnoses: cervical squamous cell carcinoma (69%) of all cervical cancers, cervical adenocarcinoma (25%) and 6% for other cervical histological cancers.
Routes of spread to other parts of the body, commonly known as metastatic sites
Cervical cancer can spread by direct extension or by lymphatic or hematogenous dissemination. Direct extension may involve the uterine corpus, vagina, parametria, peritoneal cavity, bladder, or rectum. Ovarian involvement by direct extension of cervical cancer is rare; ovarian metastases occur in approximately 0.5 percent of squamous cell carcinomas and 1.7 percent of adenocarcinomas. The most common sites for hematogenous spread are the lungs, liver, and bone; the bowel, adrenal glands, spleen, and brain are less frequent sites.
Prevention
Cervical cancer is almost preventable disease mainly by taking vaccines against HPV on time. Avoiding modifiable risk factors such as, early sexual intercourse, multiple sexual partners, smoking, and sexually transmitted diseases.
Modes of Treatment
Treatment modalities depend up on stage of the diseases.
Early stage cervical cancer: Women with cervical cancer limited to the uterus have early-stage disease. Treatment options for these women include modified radical hysterectomy, fertility-sparing surgery, or primary radiation therapy (RT) with or without chemotherapy.
Locally advanced cervical cancer
Any of the following defines the latter:
Confined to the cervix with a clinically visible tumor >4 cm (stage IB2).
Invades beyond uterus but not to pelvic wall or to lower third of vagina (stage II).
Extends to the pelvic sidewall and/or involves the lower third of vagina, and/or causes Hydronephrosis or a nonfunctioning kidney (stage III).
Invades the mucosa of the bladder or rectum, or extends beyond the true pelvis (stage IVA).
Women with locally advanced cervical cancer (stage IB2 to IVA) have a higher rate of recurrence and worse survival than those with early-stage disease (stage IA to IB1). After surgery alone, the rate of relapse is at least 30 percent, and five-year survival rates range from 80 percent for stage IB disease to 30 percent for stage III disease.
Stages used here are referred to FIGO (International Federation of Gynecology and Obstetrics) classification. Treatment for locally advanced cervical cancer consists of a combination of both chemotherapy and radiation. Almost there is no room for surgical option for management of this stage of the disease.
Metastatic cervical cancer
Cancer is said to be metastatic when it has affected sites other than primary site. In case of cervical cancer, is metastatic if any of liver, brain, bowels, bone and other organ is affected.
This stage is treated by Chemotherapy plus bevacizumab as first-line treatment. As cure and survival rates are too low, palliative care plays a major role in managing these patients.
Prognosis (Outcomes) to treatment
Prognosis is better with early stages, poorer in advanced stages.
REFERENCES :
- https://www.uptodate.com/contents/surgical-female-pelvic-anatomy
- https://www.uptodate.com/contents/
- http://www.who.int/bulletin/volumes/91/9/12-116087/en
- https://www.uptodate.com/contents/screening-for-cervical-cancer?topicRef=3179&source=see_link
- uptodate.com/contents/invasive-cervical-cancer
- https://www.sciencedirect.com/science/article/pii/S2214109X17301353
- https://www.cancer.org/cancer/cervical-cancer/detection-diagnosis-staging/staged.html
- https://www.uptodate.com/contents/management-of-locally-advanced-cervical-cancer
Researched and summarized by Dr Felix MUSABIREMA, MD working at Butaro Cancer Center of Excellence (BCCOE), Rwanda.



1 Comments
Zebadiah Martin
13 August 2019 17:03