As dengue fever is turning into a severe health crisis across the country, it is important that you know about the disease, how it spreads, and what you should do to minimize the risk of the disease.
What is Dengue?
Dengue fever is a painful, debilitating mosquito-borne disease. Aedes aegytpi, a species of mosquito, is the carrier of any one of the four closely related dengue virus serotypes -- DEN 1, DEN 2, DEN 3 and DEN 4.
The same species also causes Yellow fever, chikungunya and zika infections
A small percentage of people who had been previously infected by one of the serotypes may develop bleeding and endothelial leak if infected by another serotype which is then referred to as severe dengue or dengue hemorrhagic fever or dengue shock syndrome.
Infection with one serotype induces a lifelong immunity to the specific serotype but partial immunity to the other serotypes.
Symptoms appear between 3 to 14 days (on average 4 to 7 days) after the infective bite.
The natural course of the disease has 3 phases:
Febrile phase
Critical phase
Convalescent phase or recovery
Epidemiology
The fever is usually self limiting with a mortality of les than 1% if detected early
Dengue affects infants, young children and adults.
Prevalence of dengue is estimated to be 3.9 billion people, in 128 countries, are at risk of infection with dengue viruses.
The number of cases reported increased from 2.2 million in 2010 to over 3.34 million in 2016. Although the full global burden of the disease is uncertain, the initiation of activities to record all dengue cases partly explains the sharp increase in the number of cases reported in recent years.
Transmission
Transmitted to humans by bite of Aedes mosquito. The mosquito is usually tropical.
Individual risk factors determine the severity of the disease
These include: secondary infection, age, ethnicity and presence of chronic disease
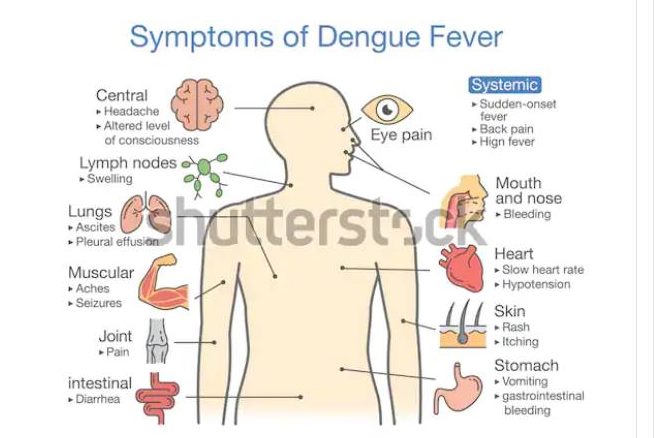
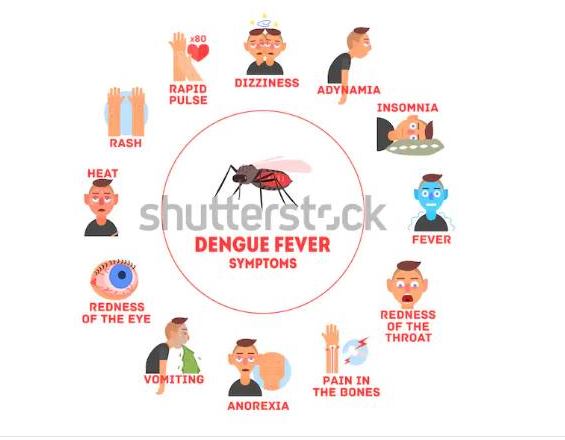
Symptoms of Dengue fever
Dengue fever has an incubation period of 3-14 days and the symptoms usually last 2-7 days.
Many individuals may however be asymptomatic.
The prodrome phase mostly consists of chills, erythematous mottling rash and facial flushing lasting 3 days.
Children less than 15 years may have a none specific febrile illness accompanied y a maculopapular rash
If one presents with the following symptoms the disease should be suspected especially if they had travelled to a highly endemic zone
Criteria for dengue
Probable dengue
Live in/ travel to endemic area
Fever and 2 of the following:
- Nausea, vomiting
- Rash, aches and pain
- Tourniquet test positive
- Leucopenia
- Any warning sighns
Warning signs
- Abdominal pain
- Persistent vomiting
- Clinical fluid accumulation
- Mucosal bleeding
- Lethargy, restlessness
- Liver enlargement> 2cm
- Laboratory increasw in H CT
Severe dengue
- Severe plasma leakage
- Severe bleeding
- Organ involvement(
Cns : impaired consciousness
Liver, kidneys
DIAGNOSIS
Laboratory criteria for diagnosis include
Demonstration of a four fold or greater change in reciprocal of IgG or IgM titre
Presence of dengue antigen in autopsy tissue via immunohistochemistry
Other work up include:
CBC
Serum protein and albumin level
Liver profile
Coagulation profile
Findings include: thrombocytopenia, leucopenia, mild to moderate elevation of aspartate aminotransferenses and alanine transferase
Severe dengue presents with: hypoproteinemia, prolonged protrombin time, increased hematocrit level, decreased fibrinogen
MANAGEMENT
SUPPORTIVE MANAGEMENT
1.Oral rehydration therapy for patients with moderate dehydration
Crystalloids ( ringers lactate, normal saline,) or volume expanders
Patients with signs of severe dengue may require admission and close monitoring of their volume status
Patients with internal bleeding may require transfusion while those with coagulopathy require fresh frozen plasma
Milk, fruit juice and oral rehydration solution can also be used
- Analgesics
Acetaminophen for fever relieve
Aspirin and other NSAIDS should be avoided
Use tepid sponging to bring down the fever in between the Paracetamol dosing. Soak a clean towel in moderately warm water, then squeeze the excess water away and wipe the body to reduce fever
- Bed rest
Patients should gradually resume normal activity during convalescence period
When to get alarmed
- Bleeding:Red spots or patches in the skin, Bleeding from nose or gums,Vomiting blood,Black colored stool,Heavy vaginal bleeding
- Frequent vomiting
- Severe abdominal pains
- Drowsiness, mental confusion or seizures
- Difficulty in breathing
Prevention and control
The main prevention technique is avoiding getting bitten by the vector by measures which include:
- preventing mosquitoes from accessing egg-laying habitats by environmental management and modification;
- disposing of solid waste properly and removing artificial man-made habitats;
- covering, emptying and cleaning of domestic water storage containers on a weekly basis;
- applying appropriate insecticides to water storage outdoor containers;
- using of personal household protection measures, such as window screens, long-sleeved clothes, repellents, insecticide treated materials, coils and vaporizers (These measures have to be observed during the day both at home and place of work since the mosquito bites during the day);
- improving community participation and mobilization for sustained vector control;
- applying insecticides as space spraying during outbreaks as one of the emergency vector-control measures;
- active monitoring and surveillance of vectors should be carried out to determine effectiveness of control interventions.
Immunization
The first dengue vaccine, Dengvaxia developed by Sanofi Pasteur was licensed in December 2015 and has now been approved in 20 countries for use in endemic areas in persons ranging from 9-45 years of age. It is given in 3 doses 0, 6 and 12 months. WHO issued a conditional recommendation on the use of the vaccine for areas in which dengue is highly endemic as defined by seroprevalence of 70% or higher. Later a retrospective study to determine serostatus at the time of vaccination were released. The analysis showed that the subset of trial participants who were inferred to be seronegative at time of first vaccination had a higher risk of more severe dengue and hospitalizations from dengue compared to unvaccinated participants.
Writer:Dr. Ishrat Rafique Eshita
REFERENCES:
1. Halstead SB. Pathogenesis of dengue: Challenges to molecular biology. Science. 1988;239:476–81.[PubMed] [Google Scholar]
2. Kurane I. Dengue hemorrhagic fever with special emphasis on immunopathogenesis. Comp Immunol Microbiol Infect Dis. 2007;30:329–40. [PubMed] [Google Scholar]
3. Gubler DJ. Dengue and dengue Hemorrhagic fever. Clin Microbiol Rev. 1998;11:480–96.[PMC free article] [PubMed] [Google Scholar]
4. New ed. Geneva, Switzerland: World Health Organization; 2009. World Health Organization (WHO). Dengue- Guidelines for Diagnosis, Treatment, Prevention and Control. [Google Scholar]
5. Guzman MG, Halstead SB, Artsob H, Buchy P, Farrar J, Gubler DJ, et al. Dengue: A continuing global threat. Nat Rev Microbiol. 2010;8(Suppl):S7–16. [PMC free article] [PubMed] [Google Scholar]
6. WHO 2009 dengue guidelines for diagnosis, treatment, prevention and control



3 Comments
�smail
28 August 2019 05:09Alexandrine
28 August 2019 05:11Zebadia Martin
01 September 2019 21:25