Diabetes mellitus is the most common metabolic disease which affects more than 170 million people worldwide, the figure being projected to 366 million by 2030 (1). In Sub-Saharan Africa, number of adult with diabetes mellitus is expected to double from 21.5 million to 41.5 million by 2035 (2). Diabetes mellitus refers to metabolic diseases sharing common phenotype of chronic hyperglycemia(3). The measure of chronic hyperglycemia is best explained by level of glycated hemoglobin i.e., HbA1c (4). Diabetes mellitus results from complex interaction between genetic and environmental factors that leads to defective or reduced insulin production due to beta cell dysfunction as seen in type 1 diabetes mellitus or decrease of glucose utilization due to insulin resistance as seen in type 2 diabetes mellitus (3). Chronic hyperglycemia which is best estimated by level of glycated hemoglobin is characterized by long term complications of diabetes mellitus which are further grouped to as vascular and non-vascular complications (3,5). Vascular complications are further grouped into macro-vascular complications, which involves large blood vessels e.g. Peripheral Arterial Diseases, stroke, ischemic heart diseases and micro-vascular complications which involves smaller blood vessel e.g. diabetic retinopathy, nephropathy and neuropathy (3,5).
Among micro-vascular complications, diabetic retinopathy is the most common and the foremost cause of blindness (3,6,7). As of 2010 this complications has affected over 100 million diabetic patients in the world and expected to rise above 190 million by 2030 (8). Development and progression of diabetic retinopathy is influenced by both ocular and systemic factors (4). Most important factors in development of diabetic retinopathy are long duration of the disease i.e., diabetes mellitus, chronic hyperglycemia and blood pressure (3,9,10). Other factors being dyslipidemia and nephropathy (11)and pregnancy (12). Chronic hyperglycemia is said to have continuous relationship with development and progression of diabetic retinopathy and thus as the level of glycated hemoglobin rises the risk also increases (4). However diabetic patients with HbA1c of less than 6.5% have minimal or no risk of diabetic retinopathy (4). Systemic high blood pressure is one of the systemic factors influencing development and progression of diabetic retinopathy although several clinical trials have shown only weak evidence (4). However some patients will not develop severe form of diabetic retinopathy even in presence of hyperglycemia, systemic arterial hypertension and other systemic factors suggesting genetic susceptibility play role in development and progression of diabetic retinopathy (11).
What happens in diabetic retinopathy?
Diabetic retinopathy is the most common diabetes mellitus micro-vascular complication which affects retinal blood vessels. The pathogenesis of diabetic retinopathy is related to prolonged exposure to hyperglycemia which is the key characteristic of diabetes mellitus (3,5). Chronic hyperglycemia which correlates with elevated glycated hemoglobin (HbA1c) is strongly associated with diabetic retinopathy (3). Several mechanism have been postulated to explain how diabetic retinopathy develops which include, increased glucose flux via alternative pathways (polyol and hexosamine pathways), activation of protein kinase C (PKC) and formation of advanced glycated end products (AGEs) (13). All these have been postulated to cause oxidative stress as a result of hyperglycemia induced mitochondrial production of reactive oxygen species i.e., super oxide formation together with pericytes dysfunction and endothelial vascular injury predispose the loss of auto-regulatory mechanism of blood-retina-barrier (BRB) which in turn there will be imbalance between the oxygen demands and perfusion. Imbalance between oxygen demand and perfusion due to loss of auto-regulatory mechanism of blood-retina-barrier (BRB) will cause ischemia and in late stages will lead to up-regulation of pro-angiogenic factors which in turn will potentiate neovascularization (5).
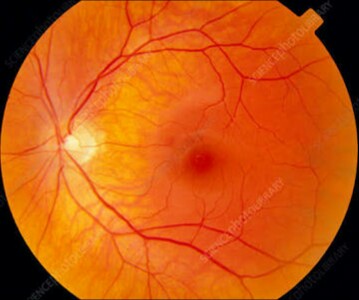
Stages of diabetic retinopathy
Diabetic retinopathy is classified into two major stages based on presence of vascular lesions and formation of new blood vessels i.e., retinal and vitreous neovascularization evident during fundoscopy or slit lamp indirect ophthalmoscopy (5). These stages are; non-proliferative diabetic retinopathy and proliferative diabetic retinopathy. Non-proliferative diabetic retinopathy becomes evident late in first decade or early in the second decade of diabetes mellitus and is characterized by presence of early retinal changes without neovascularization e.g. micro-aneurysms, blot hemorrhages, and cotton wools spots at earlier stages of non-proliferative diabetic retinopathy which may progress to advanced non-proliferative stage characterized by increase in vascular caliber, tortuosity in addition to micro-aneurysms, blot hemorrhage and cotton wools spots (3,5). In proliferative diabetic retinopathy, the hallmark is formation of new blood vessels, i.e., neovascularization in response to ischemia. Note that new blood vessels arise due to ischemic response which is characterized by up-regulation of pro-angiogenic factors e.g. vascular endothelial growth factor which potentiate neovascularization. Newly formed blood vessels doesn’t cause visual loss but predispose the retina to high risk of visual loss because newly formed blood vessels are very delicate and hence they easily rupture causing vitreous hemorrhage, fibrosis and eventually end up with retinal detachment which in turn cause complete visual loss in most cases (3).
What are challenges?
Diabetic retinopathy at earlier stages is asymptomatic and most of patients are unaware of the complication until later in advanced stages which are associated with poor vision or even sight loss. Knowledge and awareness of diabetic retinopathy is important key factor that determine response to diabetic retinopathy screening and early detection of diabetic retinopathy (14). The challenge rises in low resources settings where health workers are overwhelmed by large number of patients, e.g. smaller doctor to patient ratio. Although WHO recommends regular eye examination for every diabetic patient, response to diabetic retinopathy screening is very limited due to different factors, knowledge and awareness being important. In resource limited settings i.e., developing countries, there even limited specialist care centers where screening can be done and ophthalmologist consultation can be sought. Diabetic macular edema being the most common cause of the blindness in setting of diabetic retinopathy, its diagnosis specifically requires Optical Coherence Tomography (OCT) which in turn is not cost effective and its only limited to even fewer specialist center where majority of diabetic patients have no access.
On other hand management of diabetic retinopathy is challenging despite of good control of systemic factors. This is due to genetic factors which have been postulated in progression of diabetic retinopathy. Treatment initiation being reserved for proliferative diabetic retinopathy are Anti-vascular endothelial growth factor (Anti-VEGF) and pan-retinal photocoagulation. However most of patients are unable to afford monthly cost of Anti-VEGF injections. Thus in low resource settings most of patient will prefer pan-retinal photocoagulation because the option is cost-effective. However yet only few centers are have facilities to do so. In extreme of sight-threatening conditions such as vitreous fibrosis and retinal detachment, highly sophisticated surgeries are required while only fewer centers and retinal surgeons are available. Thus most patients with sight-threatening conditions have poor visual outcome where most of them end up to complete visual loss
Way forward
In order to improve response to diabetic retinopathy screening and follow up, knowledge and awareness have to be improved. However there must be a clear follow up plan for all diabetic patients whereby diabetic clinics have to provide clear linkage of every diabetic patient to ophthalmology clinic for regular retinal examination. This can be achieved by improving diabetic clinic sessions by incorporating important tips about diabetic retinopathy screening and follow up. Government in a particular country has a role to improve health service provision by increasing specialist centers.
It has been revealed that diabetic retinopathy is associated with chronic hyperglycemia and other systemic factors. It is thus very crucial in managing diabetics to ensure the blood glucose is tightly controlled within nearly normal ranges to reduce the risk of development and progression of diabetic retinopathy. However it is important to have effective control of other systemic risk factors such as hypertension and dyslipidemia.
Diabetic retinopathy is sight-threatening if we remain reluctant.
Writer: Zebadia Martin, a medical student at University of Dar es Salaam, Tanzania.
References
1. WHO. State of the World’s Sight. Vis 2020 Right to Sight 1999-2005. 2005;
2. International Diabetes Federation (IDF). IDF Diabetes Atlas Sixth edition, 2014 Update. IdfOrg. 2014;
3. Theodore A. Kotchen. Harrisons Principle of Internal Medicine 18th Edition. Harrisons principles of Internal Medicine. 2015.
4. Frank R. Diabetic retinopathy and systemic factors. Middle East Afr J Ophthalmol. 2015;22(2).
5. Lechner J, O’Leary OE, Stitt AW. The pathology associated with diabetic retinopathy. Vision Res. 2017;
6. Ciulla TA, Amador AG, Zinman B. Diabetic retinopathy and diabetic macular edema: Pathophysiology, screening, and novel therapies. Diabetes Care. 2003.
7. Klein BEK. Overview of epidemiologic studies of diabetic retinopathy. In: Ophthalmic Epidemiology. 2007.
8. Congdon N, Zheng Y, He M. The worldwide epidemic of diabetic retinopathy. Indian J Ophthalmol. 2012;
9. Zhang L, Krzentowski G, Albert A, Lefebvre PJ. Risk of developing retinopathy in diabetes control and complications trial type 1 diabetic patients with good or poor metabolic control. Diabetes Care. 2001;
10. Leske MC, Wu SY, Hennis A, Hyman L, Nemesure B, Yang L, et al. Hyperglycemia, blood pressure, and the 9-year incidence of diabetic retinopathy: The Barbados Eye Studies. Ophthalmology. 2005;
11. Esteves J, Laranjeira AF, Roggia MF, Dalpizol M, Scocco C, Kramer CK, et al. [Diabetic retinopathy risk factors]. Arq Bras Endocrinol Metab. 2008;
12. Axer-Siegel R, Hod M, Fink-Cohen S, Kramer M, Weinberger D, Schindel B, et al. Diabetic retinopathy during pregnancy. Ophthalmology. 1996;
13. Duh EJ, Sun JK, Stitt AW. Diabetic retinopathy: current understanding, mechanisms, and treatment strategies. JCI Insight. 2017;2(14).
14. Cleland CR, Burton MJ, Hall C, Hall A, Courtright P, Makupa WU, et al. Diabetic retinopathy in Tanzania: Prevalence and risk factors at entry into a regional screening programme. Trop Med Int Heal. 2016;21(3).



10 Comments
Fid�le
01 September 2019 19:08Zebadiah Martin
01 September 2019 19:17Mosses Evaristo
01 September 2019 19:34Kajode
01 September 2019 21:27Galus Focus
01 September 2019 23:17jackson
01 September 2019 23:50Braison cholela
02 September 2019 18:14Ngweina Magitta
03 September 2019 13:45Agapedoreen
04 September 2019 12:23Laizer,N
02 May 2020 19:15